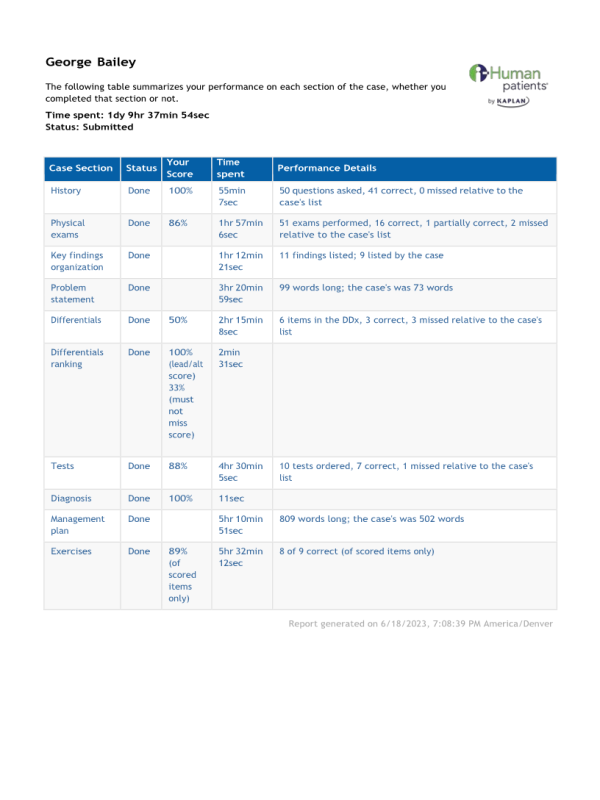
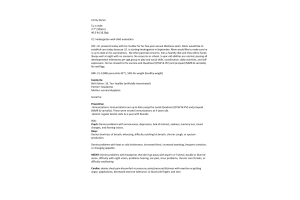
iHuman; George Bailey - Full Case
- $25.00
Problem Statement on case George Bailey
Mr. Bailey, a 62-year-old male presents to the ED with complaints of black stools with increased daily frequency and a burning upper midline epigastric pain that radiates to the back. Pain initially alleviates with food intake but worsens an hour after eating. Associated symptoms include fatigue, increased BM, and coffee-ground emesis x1.
Medications include daily intake of 81mg Aspirin P.O. and daily NSAID use (200-600mg Ibuprofen P.O.) for arthritis. Patient admits regular alcohol and tobacco use. PE is notable for orthostatic (108/80) tachycardia (92 bpm) with stable BP (122/86), scleral pallor, epigastric tenderness to palpation, and hyperactive BS 4Q.