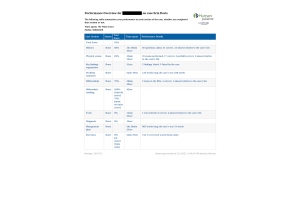
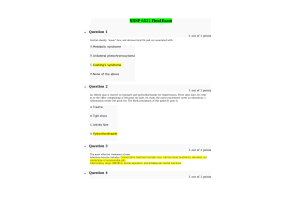
NRNP 6531 Week 6 Midterm Exam
- $45.00
- Question: Angie is a new NP who just finished her FNP program. She is having a difficult time finding an FNP position in the rural area where she lives. So, since she was an ER nurse prior to her graduate program she decides to go back to the ER as an APRN. Does she meet the competency requirements for such a position?
- Question: What is the main reason for using the REALM-SF instrument to evaluate health literacy?
- Question: A small, rural hospital is part of an Accountable Care Organization (ACO) and is ... as a Level 1 ACO. What is part of this designation?
- Question: The Consensus Model identifies 3 core courses that all ANPs must take. All the following are Advanced core courses except:
- Question: The care provided by APRNs is not limited by setting but by patient care needs.
- Question: Which is the most appropriate research design for a Level III research study?
- Question: What was an important finding of the Advisory Board survey of 2014 about primary care preferences of patients?
- Question: To reduce adverse events associated with care transitions, the Centers for Medicare and Medicaid Service have implemented which policy?
- Question: The Consensus Model for APRN regulation consists of which of the following roles?
- Question: Rules proposed by the various State Boards of Nursing must be approved by the state Legislatures.
- Question: In reviewing the Total Percentage of Body surface area for adult burn patients each, leg, arm and head are noted evaluated at 9%.
- Question: What is the initial approach when obtaining a biopsy of a potential malignant melanoma lesion?
- Question: When assisting with a skin biopsy of a patient suspected of having bullous pemphigoid (BP) lesions, what will the practitioner do?
- Question: When recommending an over-the-counter topical medication to treat a dermatologic condition, which instruction to the patient is important to enhance absorption of the drug?
- Question: Carbuncles are typically treated with systemic antibiotics
- Question: Mild acne is treated only with topicals.
- Question: Steroids should be avoided in cases of suspected fungal etiology.
- Question: A patient comes to the clinic after being splashed with boiling water while cooking. The patient has partial thickness burns on both forearms, the neck, and the chin. What will the provider do?
- Question: A provider is considering an oral contraceptive medication to treat acne in an adolescent female. Which is an important consideration when prescribing this drug?
- Question: Ashley a 24 y/o female comes to the clinic with the following chief complaint: “I have these reddish/purple raised patches all over my skin. On physical exam the NP notes that the lesions are erythematous with discrete borders that are irregular, oval or round. The most likely diagnosis based on the physical exam is:
- Question: The most common type of melanoma in African Americans and Asiansis:
- Question: Olga was making French fries for her kids and gets splashed with hot oil. At the clinic theNP notes that she has red colored skin with superficial blisters and pain where the oil splashed. The most likely diagnosisis:
- Question: Patty comes to the clinic with these soft fatty cystic lesions on her neck, trunk and arms. The most likely diagnosis is:
- Question: During a total body skin examination for skin cancer, the provider notes a raised, shiny, slightly pigmented lesion on the patient’s nose. What will the provider do?
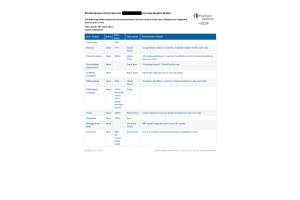
- Question: Mikey is a 19 y/o male who is brought to the clinic because he has a fever, sore throat, pain on swallowing and mildly enlarged submandibular nodes First line pharmacological treatment for Mikey would include:
- Question: During an eye examination, the provider notes a red-light reflex in one eye but not the What is the significance of this finding?
- Question: A patient diagnosed with allergic conjunctivitis and prescribed a topical antihistamine- vasoconstrictor medication reports worsening symptoms. What is the provider’s next step in managing this patient’s symptoms?
- Question: An adult patient with a history of recurrent sinusitis and allergic rhinitis reports chronic tearing in one eye, ocular discharge, and eyelid crusting. The provider suspects nasolacrimal duct obstruction. Which initial treatment will the provider recommend?
- Question: A patient diagnosed with alopecia is noted to have scaling on the affected areas of the scalp. Which confirmatory test(s) will the provider order?
- Question: A female patient is diagnosed with androgenetic alopecia. Which medication will the primary health care provider prescribe?
- Question: Mikey is a 19 y/o male who is brought to the clinic because he has a fever, sore throat, pain on swallowing and mildly enlarged sub mandibular nodes The most likely organism causing Mikey’s infection is:
- Question: Audrey is a 16 y/o female who comes to the clinic because her teacher says that she is having a hard time hearing in class. The NP examines her ears and notes that she has otitis media. If the NP performed a Weber test on Audrey she would discover that there would be:
- Question: A patient experiencing chronically dry eyes reports having a foreign body sensation, burning, and itching. A Schirmer test is abnormal. What is the suspected cause of this patient’s symptoms based on this test finding?
- Question: Which is the most common cause of orbital cellulitis in all age groups?
- Question: A patient reports bilateral burning and itching eyes for several days. The provider notes a boggy appearance to the conjunctivae, along with clear, watery discharge. The patient’s eyelids are thickened and discolored. There are no other symptoms. Which type of conjunctivitis is most likely?
- Question: A retinal detachment would be identified by a shower of floaters with the addition of sudden flashes of light.
- Question: A patient has an elevated, yellowish-white lesion adjacent to the cornea at the 3 o’clock position of the right eye. The provider notes pinkish inflammation with dilated blood vessels surrounding the lesion. What information will the provider provide the patient about this lesion?
- Question: A primary care provider may suspect cataract formation in a patient with which finding?
- Question: Aaron an 18 y/o male comes to the clinic with the following symptoms: nasal stuffiness, sneezing, scratchy irritated throat and hoarseness. He also complains of a low-grade fever and a cough that he has had for the past 4 days. Prevention of Aaron’s condition would include which of the following:
- Question: Bryce is a 17 y/o male who comes to the clinic with chief complaint of ear sudden onset of pain, popping noises, and muffled hearing. During the ear exam the NP notices that the TM has ruptured. The most likely diagnosis is:
- Question: Koplik spots on the buccal mucosa are pathognomonic for mumps.
- Question: Mikey is a 19 y/o male who is brought to the clinic because he has a fever, sore throat, pain on swallowing and mildly enlarged submandibular nodes. The most likely diagnosis for Mikey is:
- Question: A patient who works in a furniture manufacturing shop reports a sudden onset of severe eye pain while sanding a piece of wood and now has copious tearing, redness, and light sensitivity in the affected eye. On examination, the conjunctiva appears injected, but no foreign body is visualized. What is the practitioner’s next step?
- Question: A patient is seen in the clinic for patches of hair loss. The provider notes several well-demarcated patches on the scalp and eyebrows without areas of inflammation and several hairs within the patch with thinner shafts near the scalp. Based on these findings, which type of alopecia is most likely?
- Question: According to the JNC 8 guidelines the hypertension treatment goal for patients 60 years and younger should be:
- Question: An African-American patient who is being treated with a thiazide diuretic for chronic hypertension reports blurred vision and shortness of breath. The provider notes a blood pressure of 185/115. What is the recommended action for this patient?
- Question: A young adult patient is diagnosed with a mitral valve prolapse. During a routine 3-year health maintenance exam, the provider notes an apical systolic murmur and a mid-systolic click on auscultation. The patient denies chest pain, syncope, or palpitations. What action will the provider take?
- Question: A previously healthy patient presents with sudden onset of dyspnea, fatigue, and orthopnea. A family history is negative. The provider suspects myocarditis. What is the most likely etiology for this patient?
- Question: A patient is diagnosed with peripheral arterial disease (PAD) and elects not to have angioplasty after an angiogram reveals partial obstruction in lower extremity arteries. What will the provider recommend to help manage this patient’s symptoms?
- Question: A split S2 is best heard at the upper left sternum.
- Question: In coarctation of the aorta the BP of the arms is higher than the BP of the legs.
- Question: Pulsus paradoxus is a phenomenon in which the radial pulse can be palpated even though the apical pulse can’t be heard.
- Question: Juan is a known patient to the NP. He comes in for his quarterly check on his blood pressure. His blood pressure is 125/85. According to JNC 8 his BP falls into the category of:
- Question: An elderly adult patient without prior history of cardiovascular disease reports lower leg soreness and fatigue when shopping or walking in the neighborhood. The primary care provider notes decreased pedal pulses bilaterally. Which test will the provider order initially to evaluate for peripheral arterial disease based on these symptoms?
- Question: Ashley is a 47 y/o female who comes to the clinic with a chief complaint of sudden onset of palpitations and a feeling of weakness and dizziness. Additionally she notes that she has dyspnea on exertion. On the physical exam the NP notes that he HR is 120 bpm and her BP drops to 98/60. The NP after running an EKG and noting no discrete p waves and irregularly irregular rhythm diagnoses her as having:
- Question: I n performing a follow-up exam on a patient the NP discovers that the patient has a new murmur. The murmur is best heard at the apex of the heart, radiates to the axilla, and is a loud blowing and high-pitched murmur. This type of murmur is associated with which of the following conditions:
- Question: Angus is a 73 y/o male who comes to the clinic with the chief complaint of: chest pain, palpitations, exercise intolerance, intermittent periods of dizziness. Past medical records indicate that he has an enlarged heart. His diagnosis is:
- Question: A patient who is an avid long-distant runner is diagnosed with viral myocarditis. What will the provider tell this patient when asked when resuming exercising is permitted?
- Question: A patient is in clinic for evaluation of sudden onset of abdominal pain. The provider palpates a pulsatile, painful mass between the xiphoid process and the umbilicus. What is the initial action?
- Question: Dorsiflexion of the foot that produces lower leg pain is termed Homan’s Sign
- Question: Which test is diagnostic for diagnosing myocarditis?
- Question: Patients with hypertensive retinopathy will have all of the following except:
- Question: Guy is a 65 y/o male who comes to the clinic with the following chief complaint: “I have been feeling feverish, have chills, and am tired all the time. My heart also makes a funny sound.
- Question: In the physical exam the NP auscultates a heart murmur, and notices that he patient has subungual hemorrhages, petechiae on the palate, violet colored nodes on the fingers and feet, and nontender red nodes on the palms and soles of his feet. In a patient with Guy’s diagnosis, on funduscopic exam one might see:
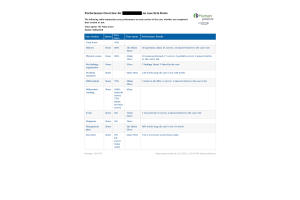
- Question: Ashley is a 47 y/o female who comes to the clinic with a chief complaint of sudden onset of palpitations and a feeling of weakness and dizziness. Additionally she notes that she has dyspnea on exertion.
- Question: On the physical exam the NP notes that he HR is 120 bpm and her BP drops to 98/60. Her EKG shows no discrete p waves and irregularly irregular rhythm. If Ashley were to start bleeding she would go to the ER and they would initiate which intervention below to reverse the effects of her war farin:
- Question: Sam is a 19 y/o male who comes to the clinic with a chief complaint of several weeks of fatigue and non-productive paroxysmal coughing. He initially had a sore throat, some rhinitis and low-grade fever. His likely diagnosis is:
- Question: Mike is a 56 y/o male who lives in an abandoned building. With about 40 other street people. He comes to the clinic with a social worker who describes his symptoms as: a cough, dyspnea, pleuritic chest pain, fever and tachypnea. Your physical exam notes that he has some consolidation in the lower lobes with an audible friction rub. Given Mike’s diagnosis the most likely causative agent is:
- Question: Artie is a 21 y/o male who comes to the clinic with a chief complaint of paroxysmal coughing without an apparent cause. He states that this has been going on for about 15 days. He initially had a mild fever, and a runny nose. First line treatment for Artie would include macrolides
- Question: Mike is a 22 y/o male who comes to your clinic with a 5-day history of cough without sputum production.
- Question: He states that his cough is worse in the morning and he has some hoarseness, post-nasal drip and a low- grade fever. Mike has otherwise been healthy Differentials for Mike might include which of the following:
- Question: A nonsmoking adult with a history of cardiovascular disease reports having a chronic cough without fever or upper airway symptoms. A chest radiograph is normal. What will the provider consider initially as the cause of this patient’s cough?
- Question: A young adult patient without a previous history of lung disease has an increased respiratory rate and reports a feeling of “not getting enough air.” The provider auscultates clear breath sounds and notes no signs of increased respiratory effort. Which diagnostic test will the provider perform initially?
- Question: Martin is a 73 y/o male who has a 50 year/pack history of smoking and comes to the clinic for his annual physical. As you are leading him back to the exam room you note that he has dyspnea with minimal cough, a barrel chest, and appears to have lost weight since his last visit. Your physical exam confirms a 20 lb. weight loss, and a more noticeable pursed lip breathing. Given Martin’s condition the first line treatment would be all the following except:
- Question: A patient with limited stage small cell lung cancer (SCLC) has undergone chemotherapy with a good initial response to therapy. What will the provider tell this patient about the prognosis for treating this disease?
- Question: Which test is the most diagnostic for chronic obstructive pulmonary disease (COPD)?
- Question: Mike is a 22 y/o male who comes to your clinic with a 5-day history of cough without sputum production. He states that his cough is worse in the morning and he has some hoarseness, post-nasal drip and a low- grade fever. Mike has otherwise been healthy Treatment for Mike’s condition would include all the following except:
- Question: Which is characteristic of obstructive bronchitis and not emphysema?
- Question: A patient diagnosed with chronic obstructive pulmonary disease reports daily symptoms of dyspnea and cough. Which medication will the primary health care provider prescribe?
- Question: A young adult patient develops a cough persisting longer than 2 months. The provider prescribes pulmonary function tests and a chest radiograph, which are normal. The patient denies abdominal complaints. There are no signs of rhinitis or sinusitis and the patientdoes nottake anymedications.What will the provider evaluate next to help determine the cause of this cough?
- Question: A patient with a smoking history of 35 pack years reports having a chronic cough with recent symptoms of pink, frothy blood on a tissue. The chest radiograph shows a possible nodule in the right upper lobe. Which diagnostic test is ... ?
- Question: A patient reports coughing up a small amount of blood after a week of cough and The patient has been previously healthy and does not smoke or work around pollutants or irritants.Whatwilltheprovidersuspectasthemostlikelycauseofthispatient’ssymptoms?
- Question: A patient reports anal pruritis and occasional bleeding with defecation. An examination of the perianal area reveals external hemorrhoids around the anal orifice as the patient is bearing down. The provider orders a colonoscopy to further evaluate this patient. What is the treatment for this patient’s symptoms?
- Question: A patient has recurrent constipation which improves with laxative use but returns when laxatives are discontinued. Which pharmacologic treatment will the provider recommend for long-term management?
- Question: Jeremy is an 18 y/o male who comes to the clinic with a chief complaint of periumbilical pain. Over the past 24 hours he has had bouts of nausea and diarrhea and pain at McBurney’s point. Which of the following diagnostic studies would be appropriate for Jeremy’s diagnosis?
- Question: Danny is a 37 y/o male who returns to the clinic for review of lab results. When he came in a week ago he complained of a “sour” taste when he belched, and severe pain in his stomach. A serum fasting gastrin level was drawn and sent to the lab. The results were 300 pg/ml. Treatment for Danny would include which of the following:
- Question: A 50-year-old, previously healthy patient has developed gastritis. What is the most likely cause of this condition?
- Question: A patient is diagnosed with fibrotic liver disease; a liver biopsy shows micronodular cirrhosis. What is the most common cause of this form of cirrhosis?
- Question: Jeremy is an 18 y/o male who comes to the clinic with a chief complaint of periumbilical pain. Over the past 24 hours he has had bouts of nausea and diarrhea and pain at McBurney’s point. The NP diagnoses him as having:
- Question: A patient experiences a feeding disorder after a stroke that causes disordered tongue function and impaired laryngeal closure. What intervention will be helpful to reduce complications in this patient?
- Question: A patient with a history of diverticular disease experiences left-sided pain and reports seeing blood in the stool. What is an important intervention for these symptoms?
- Question: A patient diagnosed with cirrhosis develops ascites. Which medication will be ordered initially to improve symptoms?
- Question: A patient with a previous history of liver disease is diagnosed with a bile duct obstruction. Which procedure will be prescribed for this patient?
- Question: Amylase and Lipase are sensitive tests used to assess for pancreatitis.
- Question: A patient with a history of diverticular disease asks what can be done to minimize acute symptoms. What will the provider recommend to this patient?
- Question: Jeremiah, a 47 y/o male presents to the clinic with episodic gastric pain he describes as gnawing and burning. He notes that the pain is temporarily relieved by food or antacids but return in full force after a couple of hours. He notes that his stools are “tarry” and he sometimes has coffee colored vomit. Jeremiah is determined to have pylori positive ulcers which treatment would be indicated?
- Question: A patient presents with fever, nausea, vomiting, anorexia, and right upper quadrant abdominal pain. An ultrasound is negative for gallstones. Which action is necessary to treat this patient’s symptoms?
- Question: Jeremiah, a 47 y/o male presents to the clinic with episodic gastric pain he describes as gnawing and burning. He notes that the pain is temporarily relieved by food or antacids but return in full force after a couple of hours. He notes that his stools are “tarry” and he sometimes has coffee colored vomit. The Gold Standard for diagnosing Jeremiah’s problem is:
- Question: A patient has sudden onset of right upper quadrant (URQ) and epigastric abdominal pain with fever, nausea, and vomiting. The emergency department provider notes yellowing of the sclerae. What is the probable cause of these findings?
- Question: An adult patient reports intermittent, crampy abdominal pain with vomiting. The provider notes marked abdominal distention and hyperactive bowel sounds. What will the provider do initially?
- Question: A patient diagnosed with chronic constipation uses polyethylene glycol and reports increased abdominal discomfort with nausea and vomiting. What is the initial action by the provider?