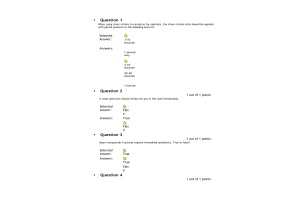
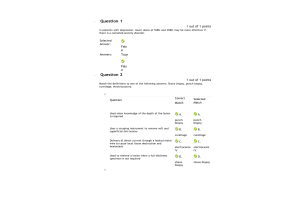
NRNP 6568 Week 6 Assignment; Assessing, Diagnosing, and Treating Patients With Complex Conditions; Pneumonia Case Study
- $20.00
Focused SOAP Note
Patient Information:
B. B., 69, M, Caucasian
S.
CC: Chest pain
HPI: This 69 y/o Caucasian male presents to the clinic for c/o chest pain. Patient reports onset “for a few days”, reports went to a large farm auction last week and started feeling sick a couple days after. Reports no one wearing masks and he admits he does not wear a mask due heat and the work he does. Describes pain as sharp and intermittent, often occurring with deep breaths.
Rates pain 8/10. Associated symptoms include fever, chills, fatigue, and productive cough which produces greenish/yellow phlegm. He admits he has not checked his temperature because he does not have a thermometer, but he has “felt hot”. States has taken Tylenol with minimal relief of pain and fever. States he has been drinking teas to try to break up the phlegm. He also reports having a decreased appetite. Denies nausea or vomiting. Denies use of antibiotics within the last 3 months.
Location: Bilateral anterior chest Onset: “for a few days”
Character: Sharp
Associated signs and symptoms: Fevers, chills, cough and fatigue Timing: Intermittent
Exacerbating/relieving factors: Deep breaths make the pain worse. Tylenol provides minimal relief
Severity: 8/10
Current Medications: No prescription medications. OTC Tylenol 500mg as needed for pain or fever. No vitamins or herbals.
Allergies: Allergies to dust and pollen. No known medication, food, or latex allergies.
PMHx: Received all immunizations as a child. Influenza vaccine 10/2020. Pneumonia vaccine “when I was in my 50’s”. Has not received any COVID-19 vaccine and has not had COVID. He
was hospitalized once for bronchitis about 35 years ago. Surgical history consists of Tonsillectomy at age 6. No blood transfusions.
Soc & Substance Hx: B B. lives in a small western Kansas community where he farms. His wife passed away 6 months ago and has 2 grown children who live on their own. He lives in the country by himself. He reports no significant health problems. Because he spends his days in the field or fixing equipment, his diet primarily consists of fast food or bologna sandwiches. Denies tobacco use or vaping, no alcohol or illicit drug use. He does keep a shot gun in the house, in an unlocked gun cabinet. He admits to never wearing a seatbelt, even on the highway. He admits he does have hand sanitizer in his truck but is not faithful about using it or washing his hands thoroughly when in hurry. No household pets. Last hearing exam was 2 years ago when he was referred by his PCP for decreased hearing; he was advised he needed hearing aids but has declined this at this time. Last dental exam was “before my wife died”. Last vision exam was “about 3 years ago”. Admits to frequent caffeine intake, consisting of 3-4 cups of coffee every morning. Tries to drink water throughout the day but often forgets because he is always “on the go”.............. Continue




























-300x200.png)