NURS 6660 Week 6 Midterm Exam (Fall Qtr)
Course : NURS 6660 Psychiatric Mental Health Nurse Practitioner Role I: Child and Adolescent
Contributed : Edwards
- $49.00
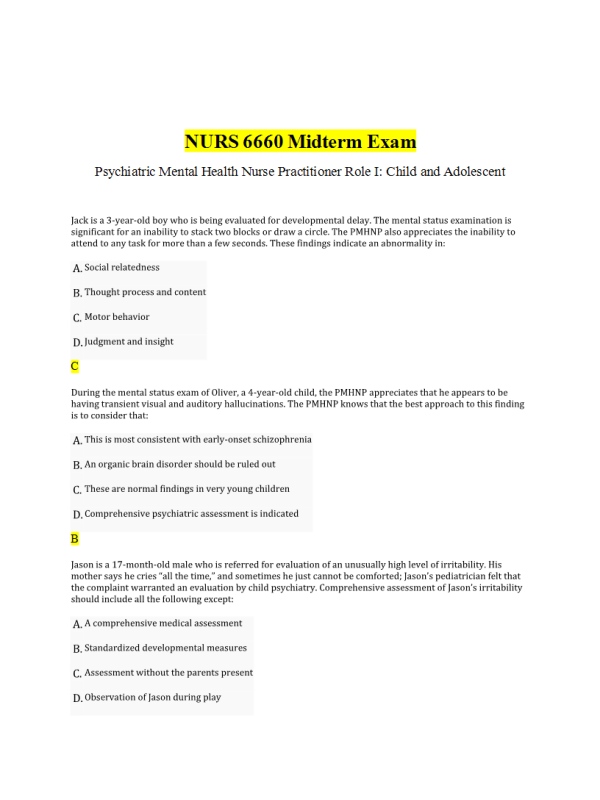
- Question: Jack is a 3-year-old boy who is being evaluated for developmental delay. The mental status examination is significant for an inability to stack two blocks or draw a circle. The PMHNP also appreciates the inability to attend to any task for more than a few seconds. These findings indicate an abnormality in:
- Question: During the mental status exam of Oliver, a 4-year-old child, the PMHNP appreciates that he appears to be having transient visual and auditory hallucinations. The PMHNP knows that the best approach to this finding is to consider that:
- Question: Jason is a 17-month-old male who is referred for evaluation of an unusually high level of irritability. His mother says he cries “all the time,” and sometimes he just cannot be comforted; Jason’s pediatrician felt that the complaint warranted an evaluation by child psychiatry. Comprehensive assessment of Jason’s irritability should include all the following except:
- Question: Which of the following is the most common anxiety disorder of childhood?
- Question: When evaluating treatment strategies for a 14-year-old patient with obsessive-compulsive disorder (OCD), the PMHNP considers that evidence-based data from the Pediatric OCD Treatment Study (POTS) suggests that best outcomes are achieved with cognitive behavioral therapy (CBT) and:
- Question: Which of the following behaviors is least suspicious for an adolescent who is being bullied at school?
- Question: Michael is a 13-year-old boy who was involved in a traumatic automobile accident in which his mother, the driver, was killed. After suffering multiple injuries and weeks in the hospital, Michael was discharged to home with physical therapy. He ultimately made a complete physical recovery but is unable to get into a car. Just the thought of riding in a car produces profound physiologic symptoms. He has been diagnosed with post-traumatic stress disorder (PTSD). His avoidance of riding in a car is conceptualized as:
- Question: Which of the following is a true statement with respect to developmental testing in infants?
- Question: Wendy is a 6-year-old female being evaluated by the PMHNP following a suicide attempt. The police were called when a neighbor saw Wendy jump out of the open window of her first-floor apartment. She was unhurt, but when the neighbor asked why she jumped out she said she wanted to kill herself. Which coincident finding would warrant an inpatient psychiatric admission for Wendy?
- Question: Caleb is a 10-year-old boy who is referred for assessment because he is not following any of the rules of discipline at home. His parents report that they have had three separate nannies resign in the last 4 months because Caleb is unmanageable. This is a long-standing problem, going back to daycare even before kindergarten. The PMHNP knows that when conducting her initial interview of Caleb she should:
- Question: Treatment of abused children is multimodal and long term. The single most important aspect of treatment is:
- Question: Psychiatric assessment of the adolescent patient is different in several ways from assessment of younger children. While trying to establish a therapeutic environment with an adolescent who is openly hostile, one of the most important things the PMHNP can do is to:
- Question: A variety of questionnaires, scales, guided-interview tools, and other standardized instruments are available to aid with various aspects of assessment. The majority are intended only to be used as an aid to information gathering and not to make a diagnosis. Which of the following tools requires training to administer and can be used to determine diagnoses?
- Question: The PMHNP is drafting a proposal for research funding for a project to offer primary prevention strategies designed to reduce the incidence of bullying. In support of this project, the PMHNP provides data supporting the fact that both perpetrators and victims of bullying suffer all of the following except:
- Question: Which of the following manifestations of childhood anxiety disorders is considered a psychiatric emergency?
- Question: The PMHNP is performing an assessment on Julie, a 4-year-old girl who has been brought to care by her mother. The mother was referred by the pediatrician because Julie has been demonstrating an appreciable change in her behavior. She is developmentally on target and has always been a happy and curious child, but for the last few months she seems to be much more fearful and anxious. Which of the following recently acquired behaviors described by the mother is most suspicious for sexual abuse?
- Question: What is the primary diagnostic difference between obsessive-compulsive disorders in children as compared to adults?
- Question: With respect to treatment of conduct disorder, the PMHNP knows that:
- Question: Kelly is a 13-year-old girl who is being evaluated because her parents are very concerned about her sudden disinterest in school. She does not want to go to any social activities and her grades have dropped markedly in the last several months. When considering bullying as a cause of her behavior change, the PMHP considers that which type of bullying is more common among girls?
- Question: Karen is a 7-year-old girl who has been started on atomoxetine 18 mg once daily for ADHD, which is just under the recommended starting dose of 0.5 mg/kg/day. After just 1 week, her parents report that she is not eating, complains of stomach pain almost every day, is having trouble sleeping, and is “really cranky.” Her teacher says she never seen anything like it; that Karen is actually worse on her ADHD medication. A careful review reveals that Karen is taking her medication just as prescribed. She is not on any other prescribed, over-the-counter, or herbal medications. The PMHNP considers that:
- Question: Carolyn is a 14-year-old female who is in care because she has developed increasingly difficult behavior at home and school. She is inappropriately dressed for the interview, wearing heavy makeup and conducting herself in a suggestive manner. Her medical history is significant only for childhood asthma and four urinary tract infections in the last year. Carolyn’s mother reveals that Carolyn’s stepfather has a history of sexually abusing his biological daughter, and the mother is beginning to wonder if something isn’t “going on” in her own home. Carolyn vigorously denies this, and indicates that her stepfather is very good to her, takes care of her, and is her “best friend.” The PMHNP recognizes that Carolyn may be in which phase of intrafamilial sexual abuse?
- Question: Phillip is a 5-year-old boy who is in care after being referred for failure to speak at school. He has been in kindergarten for 5 months, and initially his teacher thought he was just shy, so she did not focus on him. However, it has become increasingly apparent that he flat out will not speak at school. Phillip’s parents are adamant that there is not any problem at home and that Phillip talks with them and his older sister routinely. Further assessment reveals that he has always been extremely shy and that he doesn’t like it when people make a fuss over him. The PMHNP suspects that Phillip has selective mutism, which is closely related to:
- Question: With respect to psychiatric assessment, the PMNHP knows that in terms of confidentiality:
- Question: The PMHNP is performing a series of court-ordered home visits to evaluate concerns about a 4-month-old infant who presented for a well checkup with clear failure to thrive. While observing the mother’s interaction with the infant, the PMHNP notes a negative pattern of interaction. This is characterized by:
- Question: The PMHNP observes separation from and reunion with the parent as part the mental status exam of a 25-month-old toddler. Extremes of emotion during separation or reunion are most consistent with:
- Question: The PMHNP is reviewing assessment data on Richard, a 14-year-old boy who was brought in for evaluation by his parents. He has a longstanding history of being difficult, defiant, and argumentative with adults. While considering differential diagnosis of oppositional defiant disorder and conduct disorder, which of the following findings meet criteria for conduct disorder?
- Question: Melanie is a 13-month-old female who has been referred by her primary care pediatrician. She has not had consistent well-child checks, and at her first visit with this pediatrician at age 1 year, there was a notable absence of verbal babbling, interactive play, or smiling. Comprehensive assessment of Melanie must include all the following except:
- Question: Despite a wealth of data-based information on bullying, including information about its forms, presenting symptoms, and consequences, current research suggests that accurate information about bullying is not influencing preventive and awareness strategies in most school systems. When advising school personnel, parents, and primary care providers about bullying, the PMHNP should emphasize that:
- Question: Minor physical anomalies, such as high-arched palate, low-set ears, and transverse palmar creases, occur in a higher than average distribution in children with all of the following except:
- Question: Mark is a 5-year-old boy brought in for evaluation because his behavior at school has become so disruptive. According to the parents, Mark’s teacher says he just refuses to follow the rules of the classroom, openly defies her, and actually seems to try and upset his classmates. The teacher says Mark gets frustrated very easily when he cannot complete a task and is resistant to any effort to help him. This happens almost every day, and the teacher has indicated that she will not be able to keep him in the classroom if things do not change. Mark’s parents admit that he has always been “willful” and difficult to manage, but as he is an only child with a stay-at-home mom, the family overlooked his disruptive tendencies and accommodated Mark. The parents report that they often skip social events and family outings because they don’t know how Mark will behave. While counseling Mark’s parents about the theories of causation of oppositional defiant disorder (ODD), the PMHNP tells the parents that psychiatric theories include all of the following except:
- Question: Having child and adolescent patients rate their feelings and moods on a scale of 1–10 is most effective in which age group?
- Question: Which of the following is a true statement with respect to conduct disorder?
- Question: Being Brave: A Program for Coping With Anxiety for Young Children and Their Parents is a manualized intervention for anxiety disorders in young children between the ages of 4 and 7 years old. It uses a combination of parent-only and parent-child sessions and demonstrates significant improvement in children with all forms of anxiety disorders except:
- Question: Eric is an 11-year-old male for whom an emergency assessment was requested due to fire-setting. This is not Eric’s first fire, and his parents admit that he has had a bit of a fixation with the fireplace and matches for a few years. During the evaluation, the PMHNP should be particularly alert to other findings consistent with:
- Question: Which of the following is a true statement with respect to crisis intervention and psychological debriefing as a preventive strategy for post-traumatic stress disorder (PTSD)?
- Question: Which of the following is not a true statement with respect to theorized etiologies of ADHD?
- Question: The clinical interview is an important part of psychiatric assessment and should be conducted early in the diagnostic process. However, a comprehensive assessment should include other information-gathering modalities because the clinical interview:
- Question: PMHNP is evaluating a 15-year-old male patient who has been referred by his court-appointed guardian. He has been in foster care for the last 6 years and maintained a steady pattern of low-level behavior problems such as skipping school and ignoring curfew. He is not openly defiant and has always been described as a “loner.” He just does not follow most rules. During the mental status examination, the PMHNP notes that his expressions are sometimes inconsistent with the topic of conversation, and he does not seem to be able to transition effectively among levels of emotion. This represents an abnormality in:
- Question: Kevin is a 15-year-old male who presents for court-ordered psychiatric assessment. Kevin comes to his first appointment with both of his parents. He is sitting in the chair with his arms crossed and responds with “yes” and “no” answers to direct questions; otherwise, he volunteers no information. The parents are clearly upset and indicate they just “don’t know what to do with him anymore.” The most appropriate action for the PMHNP would be to:
- Question: Which of the following statements is true with respect to children who present to care acutely due to violent, enraged behavior?
- Question: Comprehensive psychiatric/mental health assessment of children includes an interview with the parents or caregivers. Which of the following is not a true statement with respect to the parental interview?
- Question: The PMHNP is evaluating his data for the assessment of Eric, a 23-month-old male who was referred because he is having nightmares to the extent that most nights he is waking up family members with his crying and screaming. In addition to the clinical interview with the parents and patient, developmental assessment, and standardized tools, the assessment should include:
- Question: Sarah is a 10-year-old patient who has been diagnosed with oppositional defiant disorder. While discussing the diagnosis, course and prognosis, and treatment strategies with Sarah’s mother, the PMHNP emphasizes that successful management of oppositional defiant disorder (ODD) must include:
- Question: Management of a child who has a pattern of fire-setting behavior must include:
- Question: The PMHNP is discussing autism spectrum disorder (ASD) treatment strategies with the parents of 4-year-old Jeffrey. He is nonverbal and has been completely unable to adapt to any changes of environment; an effort to put him in a preschool class was what precipitated his evaluation and eventual diagnosis. At this point, Jeffrey’s parents are very committed to doing anything necessary to support Jeffrey’s growth and development and promotion of prosocial behavior. While developing his plan of care, the PMHNP suggests:
- Question: Justin is a 3½ -year-old boy who comes in with his mother. She is concerned that he has obsessive-compulsive disorder (OCD). Justin’s mother says that her husband has struggled with OCD all his life; he was first diagnosed when he was 11 years old thanks to an alert teacher who suggested mental health care. Justin’s mother has been very proactive in studying genetic risk, and she knows that Justin is at significantly increased risk due to the early-onset in his father. Which of the following behaviors by Justin would be most consistent with OCD?
- Question: The PMHNP is evaluating 12-year-old Dale after the police were called to the home. Dale is assessed as having a psychotic episode; he tells the NP that voices are telling him that he is bad and that he should hurt himself. According to the mother, he has no history of psychiatric disease, medications, or really any concerns at all. Mom says he goes to school, has friends, and has always seemed “normal.” An interview with his 13-year-old sister reveals that while there is no long-term history of abnormal behavior, for the last couple of weeks things have been very strange at home. His father has been arrested for “something to do with a teenage girl,” and their parents have been fighting. His father lost his job, and there is a lot of talk about money and lawyers and jail. Dale has been very emotional as he has always been close to his Dad; he seems to go from crying to laughing in a blink, and is getting in fights at school. Even now, after he has calmed a bit, Dale’s reality testing is altered. The PMHNP considers that Dale is demonstrating:
- Question: Trauma-focused cognitive behavior therapy is a CBT approach characterized by 10–16 sessions comprised of four components: (1) psychoeducation, (2) stress inoculation, (3) gradual exposure, and (4) cognitive reprocessing. This is a management strategy for post-traumatic stress disorder (PTSD) that is:
- Question: The PMHNP is providing counseling for the family of a 6-year-old girl who was recently adopted. This girl reportedly was removed from a home in which she was subjected to severe, long-term abuse in all forms: neglect, physical abuse, sexual abuse, malnutrition, and neglect of all medical care. Upon her rescue, which was incidental during a drug raid on the home, she was hospitalized for over 1 month for physical maintenance, nutrition, hydration, and treatment for a variety of infections, including sexually transmitted diseases. The adoptive family is very committed to providing a healthy environment and is very receptive to long-term individual and family therapy. The PMHNP discusses with the new parents and siblings that which of the following is most often linked to this type of history:
- Question: Children who have been subjected to maltreatment will frequently demonstrate a variety of behavioral and psychologic symptoms, including increased aggressiveness, heightened autonomic arousal, and memory problems. Neurobiologic explanations suggest that this may be due to:
- Question: Evaluation of psychiatric emergencies in children must include:
- Question: Susan is a 10-year-old girl who has been referred by her pediatrician for mental health evaluation due to a persistent collection of somatic symptoms for which there is no apparent organic cause. For the last 2 months Susan has been increasingly distraught at the prospect of leaving home. This has become very apparent since the start of the school year. She often develops stomachaches and headaches when it is time to go to school. Lately she does not want to go to bed unless her mother remains upstairs. The PMHNP considers a diagnosis of:
- Question: While evaluating Jennifer, a 32-month-old female, for autism spectrum disorder (ASD), the PMHNP conducts a detailed assessment, including a medical history of both the patient and all first-degree family members. This is critically important as the most common known cause of ASD is:
- Question: The PMHNP has been retained by the local school board to provide comprehensive counseling and guidance following an episode of tragic school violence. A 9th grader, acting alone, brought a gun into the school, fatally shooting a teacher and injuring four other teachers and students before he was subdued. In an effort to promote best healthy practices after this traumatic event, the school board is asking for advice on how to best manage the students. The PMHNP knows that the immediate priority must be:
- Question: Comprehensive psychiatric assessment ultimately requires the integration of biological predisposition, psychodynamic factors, environmental factors, and life events. These factors, along with a mental status exam, developmental assessment, and any appropriate standardized testing is collectively referred to as:
- Question: The PMHNP is performing an emergency assessment on Renee, a 9-year-old girl who was initially brought to the attention of social services by her maternal grandmother. Renee is reluctant to talk about herself or her home life. The physical examination that accompanied this emergency assessment revealed a variety of ecchymoses in various stages of healing, and the examiner was suspicious that there was a history of sexual abuse. Renee is quiet and passive during the interview, but is rather aggressive when playing with dolls. While considering the need for removal from the home, the PMHNP knows that all the following are risk factors for predictors of further abuse and maltreatment except:
- Question: Harmony is a 4-year-old female who has been through several evaluations for behavioral abnormalities that have become increasingly disruptive, and the family is concerned for the safety of both Harmony and her 2-year-old brother. Comprehensive assessment of Harmony includes neuropsychiatric testing. The PMHNP documents the presence of neurological hard signs. These suggest:
- Question: The PMHNP is preparing an educational program for primary care providers about child abuse awareness. The goal of the program is to increase the understanding of primary care providers regarding risk factors for child abuse so that at-risk families may be identified and primary preventive strategies implemented before any harm occurs to children. The program emphasizes risk factors for child maltreatment to include all of the following except:
- Question: Kristina is a 17-year-old female who was encouraged to care by her parents because they have been worried about her. She has always been very healthy, happy, and active in school and sports. Her boyfriend of three years broke up with her last fall, right before he left for college. Since then she has lost all interest in her friends and school. Her parents say that she doesn’t do anything after school except go to her room. She has lost 16 pounds in the last 9 months. During the second session with the PMHNP, Kristina insists that her parents are overreacting, that she is doing OK in school and is eating just fine. She says of course she was sad that her boyfriend broke up with her, but she has gotten over it and moved on. During this session, the PMNHP appreciates that Kristina’s clothes are clearly too big for her, her eyes fill up with tears whenever her boyfriend is mentioned, and she does not seem engaged in the interview. While considering her assessment, the PMHNP recognizes that:
- Question: Mrs. Jacobs has accompanied her son to today’s session. Her son is in psychiatric care because he has developed disciplinary issues and for the last several months has been challenging authority, truant from school, and openly defiant of the household rules. Mrs. Jacobs is understandably distraught and is adamant that her son must be the victim of bullying because yesterday he came home from school with a black eye and a swollen lip. While this has never happened before, she believes that bullying is the only explanation for his behavior at home. While counseling Mrs. Jacobs about bullying, the PMHNP emphasizes that, by definition, bullying:
- Question: Jenny is a 5-year-old female who has been referred for consultation because the emergency room physician suspects that she might be subject to physical abuse in the home. On evaluation, the PMHNP finds Jenny to be fearful, docile, and guarded. Although clearly in pain, Jenny seems surprised when the PMHNP attempts to provide some comfort. The PMHNP notes that:
- Question: John is an 11-year-old male being evaluated for conduct disorder. His history is significant for setting fires in his neighbor’s garage, repeated episodes of truancy for the last 2 years, and three separate episodes of running away from home beginning when he was 8 years old. His teacher has reported that he is quite adept at manipulating his peers to get what he wants, and he has tried to do the same thing to her. His parents deny any concerns about anger. They are having a hard time believing that there is a problem because while John has a tendency to pursue dangerous activities, it seems more like it is just because he is bored. During interview, John does not seem at all hostile or angry. Like his parents, he does not really seem to think anything is wrong. Which of John’s findings implies the greatest risk factor for severe, persistent conduct problems?
- Question: The PMHNP is evaluating the data he has collected in the assessment of Anna, a 9-year-old girl who presented for evaluation because her teacher strongly encouraged Anna’s mother to seek care. According to the teacher, Anna has been consistently disruptive in the classroom since the beginning of the school year, 2 months ago. The assessment includes unstructured interviews with Anna, her mother, and grandmother, and Connors Parent or Teacher Rating Scale for ADHD completed by her primary school teacher and mother. The PMNHP notes a marked disparity among reports—they all seem to contradict each other. The PMHNP considers that this apparent contradiction:
- Question: Brian is a 13-year-old boy who presents for care. He was initially brought in by his mother after a family friend suggested mental health evaluation. Brian has been suffering with a variety physical symptoms for the past 8 months, ever since school started. He has missed so much school that he is in danger of not advancing to the eighth grade. He persistently complains of headache, stomachache, nausea, and dizziness. He has even vomited on more than one occasion, so his mother knows something is “really wrong.” The pediatrician has been unable to identify a cause of symptoms or offer any relief. During his interview, the PMHNP learns that this is Brian’s first year in middle school. There are hundreds of students, and it is much larger than the intimate elementary school Brian attended from kindergarten through sixth grade. Brian is certain that all the students are making fun of him; he does not even go to the lunchroom to eat. He has stopped socializing with his small group of friends from elementary school because they have made friends among the other seventh graders. Brian says he wants to have friends, but he just gets nervous and he is sure they will all make fun of him. Brian enjoys “hanging out” with his cousins, and they spent the week of spring break playing at his house. But, when it was time to go back to school, Brian was so nauseous he could not attend. Initial treatment for Brian should include:
- Question: During the initial interview with Lorraine, a 13-year-old girl being evaluated for oppositional defiant disorder (ODD), the PMHNP does not appreciate any of the behavior that has been reported by Lorraine’s mother and teachers. Lorraine is found to be well groomed, appropriate in her interaction, and says she is not sure why she is there. Lorraine says that her parents and teachers say that she is always arguing and breaking the rules, but she does not really understand what the problem is. The PMHNP notes that:
- Question: When treating anxiety disorders in young children, cognitive behavioral therapy (CBT) is preferred as initial treatment if the child is able to function sufficiently to engage in daily activities while in treatment. Which of the following therapies is appropriate for those children too young to engage in traditional CBT?
- Question: Adam is a 26-month-old boy referred by his pediatrician for evaluation of speech delay. He has not spoken any intelligible words. Adam is an only child, and the parents deny any contributory medical history. Adam was delivered at 38 weeks 5 days’ gestation without complication. At 5 weeks of age he developed respiratory failure due to respiratory syncytial virus (RSV) and was hospitalized on a ventilator for several days; since then, the parents report only the occasional upper respiratory virus. They report that Adam is a “really good” child and will often entertain himself for periods of time with his building blocks; rarely he will have a “temper tantrum.” The parents confirm that Adam does not speak any recognizable words. While he does make sounds, his parents admit that he does not appear to be trying to communicate with them. When considering a diagnosis of autism spectrum disorder (ASD), the PMNHP would expect further history and examination to reveal:
- Question: Nate is a 9-year-old boy who presents for a follow-up visit. He was diagnosed with ADHD 4 months ago and started on methylphenidate 5 mg b.i.d. At a 1-month follow-up his mother reported that he was not really demonstrating any improvement of symptoms, so he was increased to 10 mg b.i.d. He has been on this dose for 1 month. Nate reports that sometimes he doesn’t feel so great; he gets a stomach ache sometimes and a few weeks ago he felt “dizzy.” His vital signs are within normal limits. Mom says that on this dose his teacher says his behavior in school is much improved, and she notices that at home he seems more focused and is able to do his homework and chores. The appropriate action with regard to his medications at this point would be to:
- Question: Because some children exposed to significant traumatic events do not develop post-traumatic stress disorder (PTSD), there has been research interest in neurobiology and assessment of predisposing or risk factors. Children with PTSD have been noted to have which of the following when compared to age-matched controls?
- Question: The PMHNP is writing an article to increase awareness among pediatric primary care providers to those factors that may suggest higher than average risk for the development of childhood anxiety disorders. It is helpful to note that which of the following are neurophysiologic correlates between young children and anxiety disorders?
- Question: Richard is an 11-year-old patient who has been hospitalized following a suicide attempt in which he mixed a variety of household cleansers and poisons and swallowed them. He has been medically cleared, and his initial psychiatric assessment reveals a preadolescent male who made this suicide attempt because he was so unhappy at school. His family recently moved from another part of the country and he started a new school. The other children have been bullying him, and he just decided it would be better to die. He has no siblings and no friends in this new town. Which additional findings during this assessment would prompt the PMHNP to suggest a psychiatric admission?
- Question: Kelly is an 8-year-old girl who is being evaluated by the PMHNP because she is markedly behind her peers in school performance. During her mental status examination, she is unable to repeat three objects after five minutes, and is unable to repeat five digits forward or three digits backward. Further evaluation reveals an inability to add single digits. The PMHNP interprets this finding as:
- Question: A variety of diagnostic instruments are available to assist the PMHNP with comprehensive data collection. Which of the following tools is considered an “interviewer-based” tool designed as a guide to clinicians designed to help clarify answers to questions?
- Question: Psychiatric assessment of children and adolescents is best achieved by a combination of tools and techniques best suited to the child’s age and developmental stage. When interviewing a 10-year-old, the PMHNP may have the best success by having the patient: