PRAC 6665 Week 3 Assignment 2; Focused SOAP Note and Patient Case Presentation
- $15.00
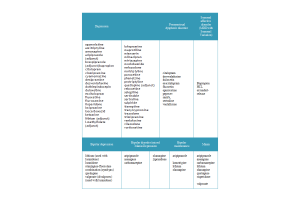
Week 3: Focused SOAP Note and Patient Case Presentation College of Nursing-PMHNP, Walden University NRNP 6665: PMHNP Care Across the Lifespan 1 Practicum Introduction Every patient's treatment begins with a full health assessment, because the plan of care and every mental intervention are all dependent on the information gathered at the initial meeting with the patient. In this situation, the assessment was documented after the patient was evaluated, and a diagnostic impression was formed based on the information gained from the patient during the evaluation. A 30 years old White female attending a follow up on tele psych appointment. Patient states that she is doing well with meds. Patient is taking all prescribed medications: Gabapentin 100mg PO 3 times per day, Wellbutrin 300mg PO daily, Effexor 112mg PO daily and will continue with the above listed medications as they are effective. Subjective: CC: "Sometimes I get really anxious, sometimes depressed. It's hard to describe my feelings". HPI: Amy a 30 years old White female attending a follow up on tele psych appointment. Patient states that she is doing well with meds. Patient is taking Gabapentin 100mg PO 3 times per day, Wellbutrin 300mg PO daily, Effexor 112mg PO daily. Patient admits to the use of Weed and Alcohol daily. Admits that she took alcohol last night and that has been going on for the last 10 days. States that weed makes her more social, calm, get things done. The patient was evaluated by the Nurse Practitioner student. The patient describes her mood as good. Her affect is restricted but adequate. Patient denies SI/HI. Following the note on prior meeting with patient and the psychiatrist, patient is coping well with her mental condition. Substance Current Use and History: Patient admit to use of alcohol and weed. Admits that she took alcohol last night and that has been going on for the last 10 days. States that weed makes her more social, calm, get things done. Medical History: Patient denies any medical history Current Medication: Gabapentin 100mg PO 3 times per day, Wellbutrin 300mg PO daily, Effexor 112mg PO daily Allergies: No known drug allergies, food or seasonal allergies Reproductive History: Patient is presently sexually active, practices safe sex. No history of abortion or miscarriages ROS: GENERAL: Well attired, appeared nervous and shy during the session. HEENT: There is no swelling or redness in the eyes. Denies having an ear condition. No abnormalities or disfigurements were found in the nose. There is no deviation or swelling in the throat or neck. SKIN: no discoloration noted or history of skin condition CARDIOVASCULAR: Within typical limits for heart rate and blood pressure PULMONARY: There are no aberrant noises in any of the lungs; sounds all clear GASTROINTESTINAL: able to move bowels without no problem or discomfort GENITOURINARY: continent times two......... Continue